

SLEEP APNEA INFORMATION
Sleep apnea is a serious, potentially life-threatening condition that is far more
common than generally understood. First described in 1965, sleep apnea is a
breathing disorder characterized by brief interruptions of breathing during
sleep. It owes its name to a Greek word, apnea, meaning “want of breath.” There
are two types of sleep apnea: central and obstructive. Central sleep apnea,
which is less common, occurs when the brain fails to send the appropriate signals
to the breathing muscles to initiate respirations. Obstructive sleep apnea is
far more common and occurs when air cannot flow into or out of the person’s
nose or mouth although efforts to breathe continue.
In a given night, the number of
involuntary breathing pauses or “apneic events” may be as high as 20 to 60 or
more per hour. These breathing pauses are almost always accompanied by snoring
between apnea episodes, although not everyone who snores has this condition.
Sleep apnea can also be characterized by gasping or choking sensations. When
breathing stops, the sleeper is awakened just enough to inhale and resume
breathing, often without being aware of the sleep disruption. In fact, many
people with sleep apnea may be unaware of the problem. The frequent
interruptions of deep, restorative sleep often leads to excessive daytime
sleepiness and may be associated with an early morning headache.
Early recognition and treatment of
sleep apnea is important because it may be associated with irregular heartbeat,
high blood pressure, heart attack, and stroke.
Sleep apnea occurs in all age groups and both sexes but is more common in men (it may be
underdiagnosed in women), people over 40 years of age and possibly young
African Americans. It has been estimated that as many as 18 million Americans
have sleep apnea. Four percent of middle-aged men and 2 percent of middle-aged
women have sleep apnea along with excessive daytime sleepiness. People most
likely to have or develop sleep apnea include those who snore loudly and also
are overweight, or have high blood pressure, or have some physical abnormality
in the nose, throat, or other parts of the upper airway. Sleep apnea seems to
run in some families, suggesting a possible genetic basis.
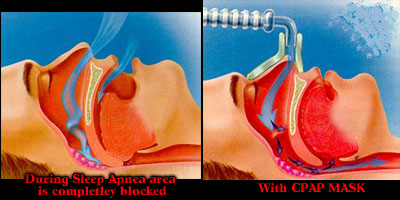
Certain mechanical and structural problems in the airway cause the interruptions in breathing
during sleep. In some people, apnea occurs when the throat muscles and tongue
relax during sleep and partially block the opening of the airway. When the
muscles of the soft palate at the base of the tongue and the uvula (the small
fleshy tissue hanging from the center of the back of the throat) relax and sag,
the airway becomes blocked, making breathing labored and noisy and even
stopping it altogether. Sleep apnea also can occur in obese people when an
excess amount of tissue in the airway causes it to be narrowed. With a narrowed
airway, the person continues his or her efforts to breathe, but air cannot
easily flow into or out of the nose or mouth. Unknown to the person, this
results in heavy snoring, periods of no breathing, and frequent arousals
(causing abrupt changes from deep sleep to light sleep). Ingestion of alcohol
and sleeping pills increases the frequency and duration of breathing pauses in
people with sleep apnea.
Note:
Researchers are still unsure about the cause and effect
relationship between sleep apnea and other disorders, but there is a clear
association between the OSA and conditions like hypertension, heart disease,
stroke, ulcers and more.
http://usmedicine.com/article.cfm?articleID=678&issueID=51
I believe that my Sleep Apnea is caused by
one or more of the following:
Hypertension, Diabetes Type II, PTSD and/or
Nasal problems and I will be writing up my VA claim in this manner.
During the apneic event, the person is unable to breathe in oxygen and to exhale
carbon dioxide, resulting in low levels of oxygen and increased levels of
carbon dioxide in the blood. The reduction in oxygen and increase in carbon
dioxide alert the brain to resume breathing and cause an arousal. With each
arousal, a signal is sent from the brain to the upper airway muscles to open
the airway; breathing is resumed, often with a loud snort or gasp. Frequent
arousals, although necessary for breathing to restart, prevent the patient from
getting enough restorative, deep sleep.
Because of the serious disturbances in their normal sleep patterns, people with sleep
apnea often feel very sleepy during the day and their concentration and daytime
performance suffer. The consequences of sleep apnea range from annoying to
life-threatening. They include symptoms suggesting depression, irritability,
sexual dysfunction, learning and memory difficulties, and falling asleep while
at work, on the phone, or driving. Untreated sleep apnea patients are 3 times
(or more) likely to have automobile accidents; CPAP treatment reverses the
increased risk. It has been estimated that up to 50 percent of sleep apnea
patients have high blood pressure. It has recently been shown that sleep apnea
contributes to high blood pressure. Risk for heart attack and stroke may also
increase in those with sleep apnea.
For many sleep apnea patients, their bed partners or family members are the first
ones to suspect that something is wrong, usually from their heavy snoring and
apparent struggle to breathe. Coworkers or friends of the sleep apnea victim
may notice that the individual falls asleep during the day at inappropriate
times (such as while driving a car, working, or talking). The patient often
does not know he or she has a problem and may not believe it when told. It is
important that the person see a doctor for evaluation of the sleep problem.
In addition to the primary care physician, pulmonologists, neurologists, or other
physicians with specialty training in sleep disorders may be involved in making
a definitive diagnosis and initiating treatment. Diagnosis of sleep apnea is
not simple because there can be many different reasons for disturbed sleep.
Several tests are available for evaluating a person for sleep apnea.
Polysomnography is a test that records a variety of body functions during sleep, such as
the electrical activity of the brain, eye movement, muscle activity, heart
rate, respiratory effort, air flow, and blood oxygen levels. These tests are
used both to diagnose sleep apnea and to determine its severity.
The Multiple Sleep Latency
Test (MSLT) measures the speed of falling asleep.
In this test, patients are given several opportunities to fall asleep during
the course of a day when they would normally be awake. For each opportunity,
time to fall asleep is measured. Individuals who fall asleep in less than 5
minutes are likely to require some type of treatment for sleep disorders. The
MSLT may be useful to measure the degree of excessive daytime sleepiness and to
rule out other types of sleep disorders.
Diagnostic tests usually are performed
in a sleep disorders center, but new technology may allow some sleep studies to
be conducted in the patient’s home.
The specific therapy for sleep apnea is tailored to the individual patient based on medical
history, physical examination, and the results of polysomnography. Medications
are generally not effective in the treatment of sleep apnea. Oxygen is
sometimes used in patients with central apnea caused by heart failure. It is
not used to treat obstructive sleep apnea.
Nasal continuous positive airway pressure (CPAP) is the most
common effective treatment for sleep apnea. In this procedure, the patient
wears a mask over the nose during sleep, and pressure from an air blower forces
air through the nasal passages. The air pressure is adjusted so that it is just
enough to prevent the throat from collapsing during sleep. The pressure is
constant and continuous. Nasal CPAP prevents airway closure while in use, but
apnea episodes return when CPAP is stopped or it is used improperly.
Variations of the CPAP device attempt
to minimize side effects that sometimes occur, such as nasal irritation and
drying, facial skin irritation, abdominal bloating, mask leaks, sore eyes, and
headaches. Some versions of CPAP vary the pressure to coincide with the
person’s breathing pattern, and other CPAPs start with low pressure, slowly
increasing it to allow the person to fall asleep before the full prescribed
pressure is applied.
Dental appliances that reposition the lower jaw and the tongue have been helpful to some
patients with mild to moderate sleep apnea or who snore but do not have apnea.
A dentist or orthodontist is often the one to fit the patient with such a
device.
Some patients with sleep apnea may need
surgery. Although several surgical procedures are used to increase the size of
the airway, none of them is completely successful or without risks. More than
one procedure may need to be tried before the patient realizes any benefits.
Some of the more common procedures
include removal of adenoids and tonsils (especially in children), nasal polyps
or other growths, or other tissue in the airway and correction of structural
deformities. Younger patients seem to benefit from these surgical procedures
more than older patients.
Uvulopalatopharyngoplasty (UPPP) is a procedure used to remove excess tissue at the back of the
throat (tonsils, uvula, and part of the soft palate). The success of this
technique may range from 30 to 60 percent. The long-term side effects and
benefits are not known, and it is difficult to predict which patients will do
well with this procedure.
Laser-assisted
uvulopalatoplasty (LAUP) is done to eliminate snoring
but has not been shown to be effective in treating sleep apnea. This procedure
involves using a laser device to eliminate tissue in the back of the throat.
Like UPPP, LAUP may decrease or eliminate snoring but not eliminate sleep apnea
itself. Elimination of snoring, the primary symptom of sleep apnea, without
influencing the condition may carry the risk of delaying the diagnosis and
possible treatment of sleep apnea in patients who elect to have LAUP. To
identify possible underlying sleep apnea, sleep studies are usually required
before LAUP is performed.
Somnoplasty is a procedure that uses
radiowaves to reduce the size of some airway structures such as the uvula and
the back of the tongue. This technique is being investigated as a treatment for
apnea.
Tracheostomy is used in persons with severe, life-threatening sleep apnea. In this
procedure, a small hole is made in the windpipe and a tube is inserted into the
opening. This tube stays closed during waking hours, and the person breathes and
speaks normally. It is opened for sleep so that air flows directly into the
lungs, bypassing any upper airway obstruction. Although this procedure is
highly effective, it is an extreme measure that is rarely used.
Other procedures: Patients in whom sleep apnea is due to deformities of the lower jaw may
benefit from surgical reconstruction. Finally, surgical procedures to treat
obesity are sometimes recommended for sleep apnea patients who are morbidly
obese.
Behavioral changes are an important
part of the treatment program, and in mild cases behavioral therapy may be all
that is needed. Overweight persons can benefit from losing weight. Even a 10
percent weight loss can reduce the number of apneic events for most patients.
Individuals with apnea should avoid the use of alcohol, tobacco and sleeping
pills, which make the airway more likely to collapse during sleep and prolong
the apneic periods. In some patients with mild sleep apnea, breathing pauses
occur only when they sleep on their backs. In such cases, using pillows and
other devices that help them sleep in a side position may be helpful.
If you are experiencing sleepiness during the day, loud snoring or pauses in breathing during
sleep or any other sleeping difficulties, make an appointment to discuss these
problems with your doctor. Sleep disorders are treatable. Your doctor can
evaluate your sleep problem and may refer you to a sleep specialist who has
special training in sleep medicine. Many of these specialists work at sleep
centers where overnight sleep studies can help determine whether you have a
sleep disorder.
Of 1,022 patients in a recent study, those who had obstructive
sleep apnea were twice as likely to have a stroke or die from any cause during
the 3.5-year follow-up period. In sleep apnea, the upper airway closes
repeatedly during sleep. The disorder had been linked in prior research to a
higher risk of stroke and other cardiovascular diseases, but researchers
weren't sure if this was only because those with sleep apnea were also more
likely to have other risk factors, such as obesity or high blood pressure. In
the new study, researchers from the VA Connecticut Healthcare System and Yale
University School of Medicine determined that the connection between sleep
apnea and stroke persists even independent of other risk factors.
Yaggi
HK, Concato J, Kernan WN, Lichtman JH, Brass LM, Mohsenin V.
Obstructive sleep apnea as a risk factor for stroke and
death. N Engl
J Med. 2005 Nov 10;353(19):2034-41.
| Sleep Apnea Links | |
|---|---|
| American Sleep Apnea Association | http://www.sleepapnea.org/ |
| National Sleep Foundation | http://www.sleepfoundation.org/sleepcenters/locate.php?state=VA |
| VA Tackles Rising Rates Of Sleep Apnea | http://usmedicine.com/article.cfm?articleID=678&issueID=51 |
| The Sleep Channel | http://www.sleepdisorderchannel.net/osa/ |
| HelpGuide on Sleep Apnea | http://www.helpguide.org/life/sleep_apnea.htm |
